Case Study 3
Focus on Days Revenue Outstanding
Profile: Two Physician Practice Group
Problem Prior to Engaging Integra MDP
Integra MDP Action Plan
Initial analysis identified a lack of automation in claims submission and management coupled with a minimal utilization of ACH/EFT reciting structures.

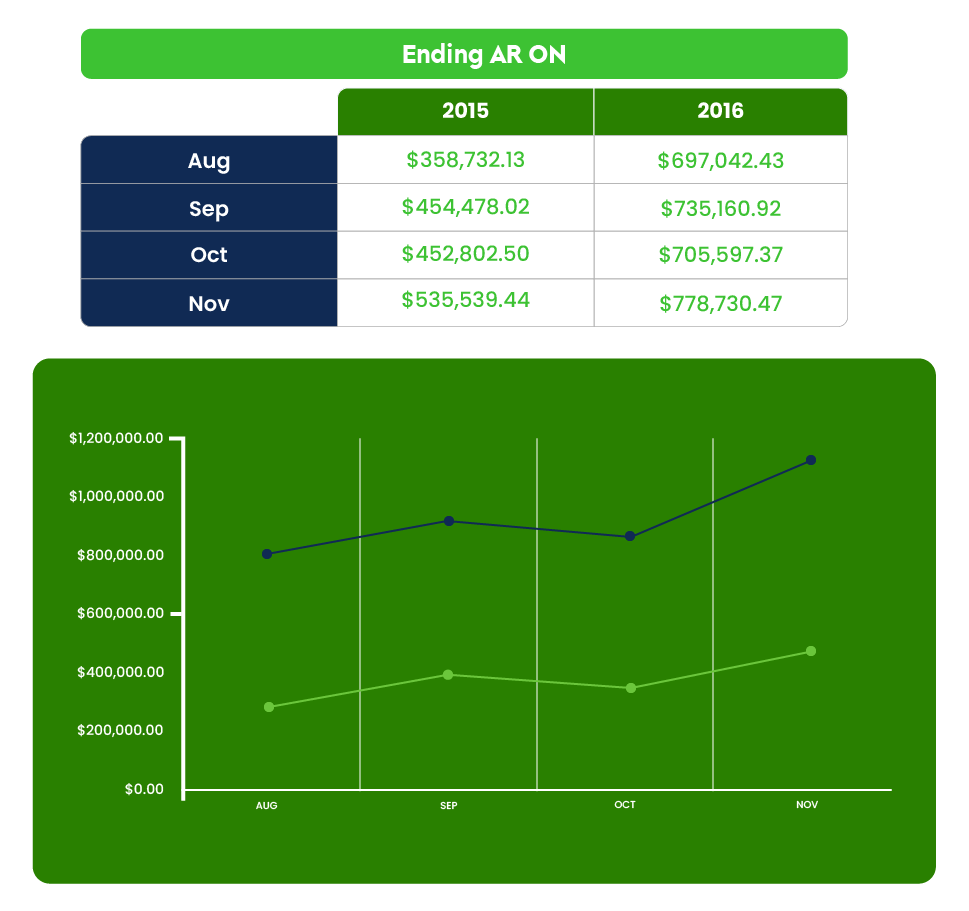
A thirty day action plan was developed and implemented to address the structural issues faced by the practice. Specific, Measurable & Actionable items were tracked and reported through Integra’s Client Portal with Key Performance Measurement Dashboards depicting real-time results. Results were discussed with the Practice Leaders during monthly business meetings along with newly identified performance improvement initiatives uncovered during the prior month.
End Result
• After 6 months, 90% of all claims were closed within 30 days of the date of the encounter.
• Real revenue adjusted for patient volume increased by 6% over the same period