Case Study 2
Focusing on Insurance Contract Problems
Profile: Multi Location Urgent Care Group
Problem Prior to Engaging Integra MDP
Integra MDP Action Plan
Integra immediately identified the non-compliant providers and managed the practice group team in closing all credentialing efforts. Further, we recommended changes to the new hire process for the group to better manage credentialing. Additionally, we worked with the client team to instill processes that segregated providers to patient groups for which they were compliant (Medicare vs. Commercial/Self).

On a parallel track, contracts were updated with each expired payer and new contracts were executed based on utilization reports which identified out of network payer patient volume trends.
A thirty day action plan was developed and implemented to address the structural issues faced by the practice. Specific, Measurable & Actionable items were tracked and reported through Integra’s Client Portal with Key Performance Measurement Dashboards depicting real-time results. Results were discussed with the Practice Leaders during monthly business meetings along with newly identified performance improvement initiatives uncovered during the prior month.
Above core changes were completed within 4 months.
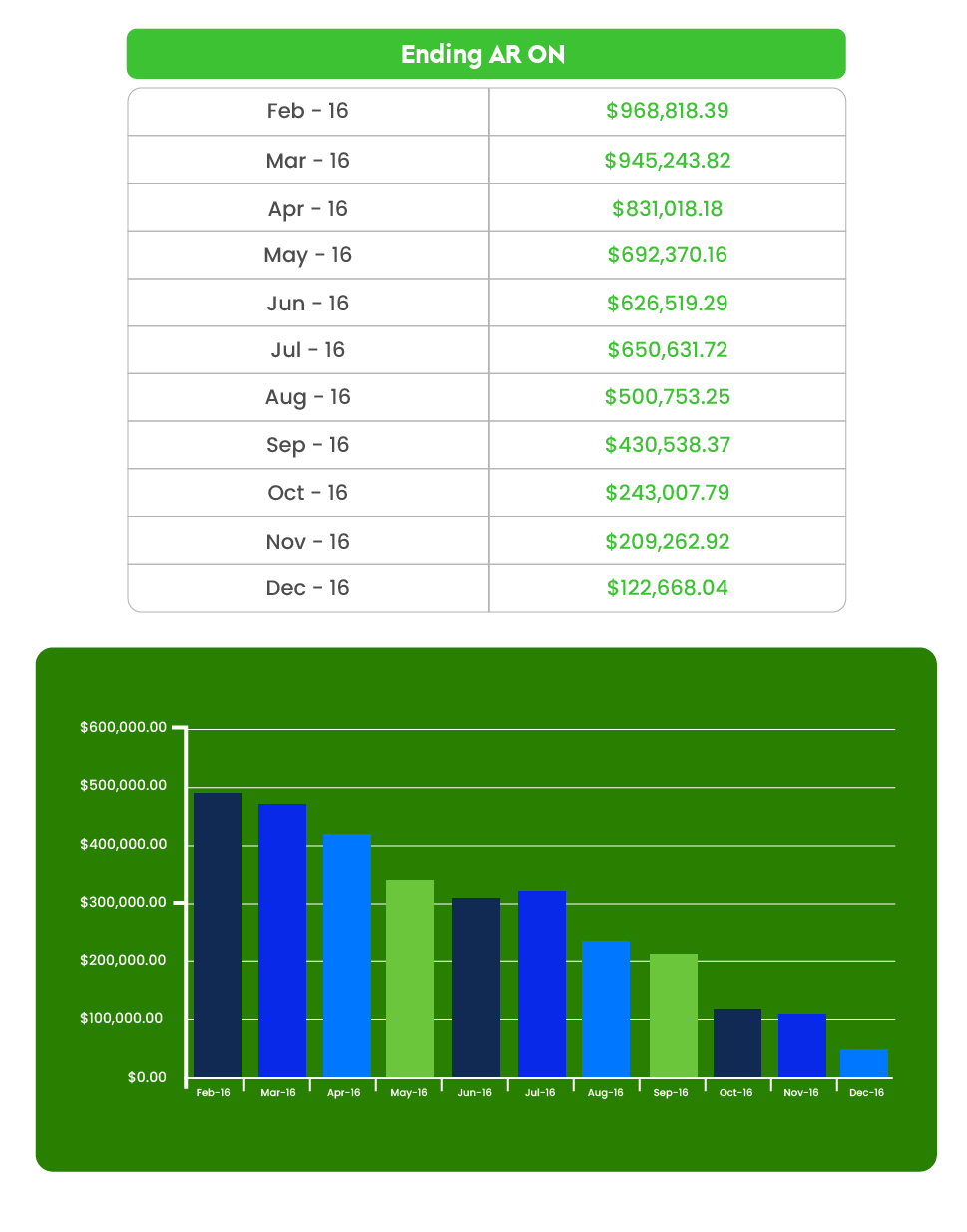
End Result
• After 6 months, 90% of all claims were closed within 30 days of the date of the encounter.
• Days Revenue Outstanding (measurement of time between patient encounter to first insurance dollar received) reduced by 71% over the first 6 months